Precision oncology paired with real-world data and just-in-time enrollment strategies is the new paradigm in oncology treatment. Wider access to patient genomic data and to AI tools allows us to not only design novel treatments but match them to the patients most likely to benefit.
Recursion is actively leveraging the power of its AI-driven phenomics platform – along with other forms of data, including genetic and real world patient data – to discover new ways to target aggressive cancers and identify biomarkers that can better guide patient selection and improve outcomes.
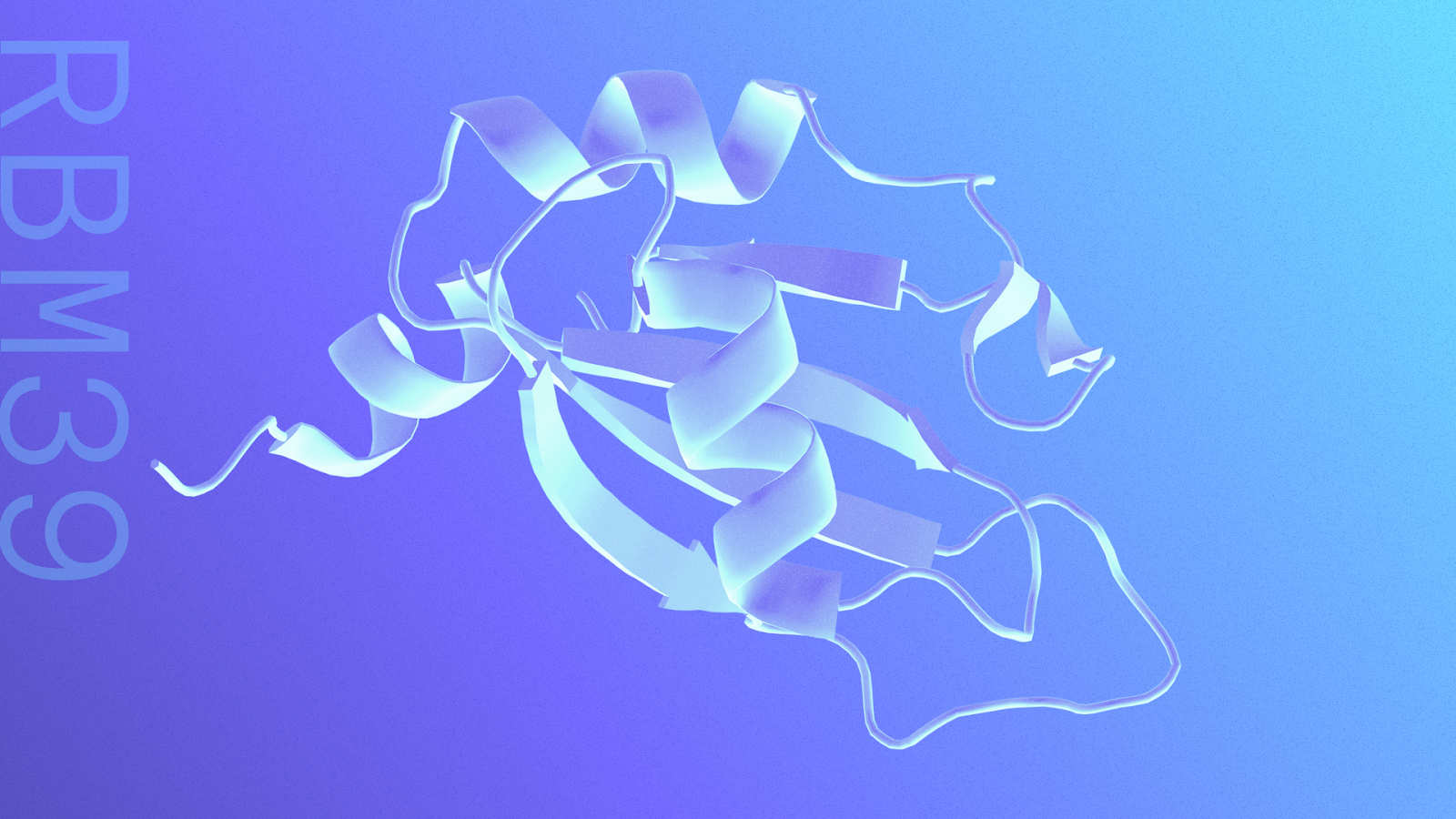
Back in 2021, scientists using the Recursion OS (then in its 1.0 version) made an exciting discovery. Exploring the maps of biology built on the company’s automated lab-generated phenomics data, they found that the splicing factor protein RBM39 (related to turning genes into proteins) was associated with key regulators of DNA damage response (DDR). In fact, degrading RBM39, they discovered, would have the same effect as inhibiting a highly desirable cancer target, CDK12. But unlike CDK12, targeting RBM39 would not also inhibit CDK13 and lead to toxic side effects. This is a prevailing theme for Recursion’s phenomics-enabled programs – to identify novel targets by inference that influence well described areas of biology with clear clinical relevance as potential differentiated first-in-class opportunities.
For RBM39, the program team used the same AI platform for discovery – both optimizing chemistry and improving chemical properties – in order to design the potentially first-in-class degrader REC-1245. The molecule is optimized to target RBM39 without directly impacting CDK12 or CDK13 activity. Preclinical studies validated the discovery – showing that RBM39 degradation induces splicing defects which lead to DNA damage, and subsequent cell cycle arrest in the right context. Thanks to the efficiency of the platform, which allows for virtual modeling and scoring of molecules, only the most promising compounds were synthesized. As a result, the process from biological discovery to lead drug candidate happened in under 18 months, more than twice the speed of industry average.
“A year and a half before others discovered it, we had already observed the relationship between RBM39 and DNA damage response and also demonstrated the in vivo proof of concept,” says @Chase Neumann, PhD, associate director of oncology at Recursion and one of the scientists involved. “The inference map discovery was amazing to see, but as a scientist I'm naturally skeptical. Seeing that proof of concept play out in vivo was when it really was exciting.”
It’s no secret that 90% of drugs fail in clinical trials – most often due to lack of efficacy. When it comes to cancer, a “one size fits all” treatment approach won’t work, because not all cancers of the same type are identical. Predictive biomarkers such as genetic mutations help to predict which patients with a cancer type are most likely to respond to a specific drug.
For instance, just 5% of non-small cell lung cancer patients have a genetic mutation driven by anaplastic lymphoma receptor tyrosine kinase (ALK+) and will benefit from drugs that block that gene. Just 20% of breast cancer patients will benefit from drugs targeting the HER2 protein. One of the most famous and earliest examples of a precision cancer treatment was the drug Gleevec, a selective BCR-ABL1 kinase inhibitor approved in 2001 for the treatment of chronic myelogenous leukemia (CML), a rare form of cancer that affects certain white blood cells. In 2017, a long-term study found that patients taking the drug for more than 10 years had an overall survival rate of over 83%. Precision oncology works.
“Moving from paradigms of cancer as a singular disease, precision oncology today seeks to select patients based on underlying characteristics including mutations and other genomic features,” Neumann says. “The field is building toward identifying patients earlier to direct treatment plans to improve patient outcomes sooner. Today, the near expectation within clinical trial design includes a focus on identifying the right patient as early as possible.”
In the case of REC-1245, experiments to inform patient selection efforts screened a large collection of cancer models from the Cancer Cell Line Encyclopedia – a resource from the @Broad Institute and @Novartis which provides open access to genomic data for nearly 1,000 cancer cell lines. They looked for specific shared genetic characteristics – known as biomarkers – associated with a cancer model's response to the drug.
They found, among many positive signals, better responses in patient models that had genomic instability characterized by replication stress and DNA repair vulnerabilities (DDR defects) - where the normal DNA repair systems aren’t working correctly — including Microsatellite instability-high (MSI-high) and Homologous recombination repair (HRR) altered cancers. Recursion used these clinical relevant biomarkers to select patients for the DAHLIA clinical trial.
Applying additional cancer patient data from partners, researchers are identifying patients with those relevant mutations who are most likely to respond to REC-1245 and who would be eligible to enroll in the trial. “Our drug response is tied to a predictive biomarker that we can then enrich clinically,” Neumann says.
Today, REC-1245 is advancing in Phase 1/2 trials using the biomarkers above to enrich the patient population, including patients with certain solid tumors or lymphoma.
And Recursion has now integrated patient data at every stage of the drug discovery and development process, including identifying biomarker strategies and training causal AI models to initiate new drug programs.
“We pick a patient context based on genetic driver mutations and then we look at whether we have the novel chemistry and/or biology insights there that no one else has seen,” Neumann says.
Written by: Brita Belli, Senior Communications Manager, Recursion